Actually no, as many already knew South Korean Women are Superior.
And they on average are not taller than in the "Western" World.
This is a reply to someone claiming taller women are superior according to "Science". Some people read and quote selectively, most likely because Ideology, lack of experience and lack of training. Lack of relevant expertise in the field of the data they parrot. Quack! Quack!: Ugly ducklings, Canards...
--"Common sense is the least common of senses". Paraphrasing Voltaire.
Re: "Predicting mid-pelvic interspinous distance in women using height and pubic arch angle"
I do not authorize psychological nor psychiatric formulations, interpretations nor diagnosis, etc. I do not authorize any Religious use of my texts. Rights Reserved. This is not medical advice nor advice of any kind. This is a debunking effort not a statement. I dedicate this Post of mine to Choa Park, Kim Seol-hyun, Kwon Mina and Seo Yu-na, former members of the South Korean Female Band AoA, Ace of Angels.
It was a common dictum that non-pregnant measurements of the bony birth canal were of little use to predict delivery complications for "cephalo-pelvic" dystocias.
Hence the study of MRI you quote most likely won´t have a predictive value in practice.
In old practice pelvic measurements were done close to delivery because it was believed until then they had no predictive value.
Supported in the quoted study by this:
"Pelvic capacity is greater at 32 weeks than at 20 weeks;"
Then it evolve to abandon clinical measurements and X ray studies. Those had no value either in routine practice.
From my experience, but it does say this:
"We measured women’s parameters according to reproductive age because the bone structure, which acts as a passage during delivery, does not change significantly during reproductive age"
And the interspinous difference was measured by regression, it was estimated, it was not measured directly as a predictive variable:
"Two significant regression formulas for predicting ISD were identified as follows: ISD = 0.24973 × height − 0.06724 × inlet-AP distance + 0.12166 × outlet-AP distance + 0.29233 × ischial tuberosity distance + 0.32524 × PAA (P < 0.001, R2 = 0.9973 [adjusted R2 = 0.9973]) and ISD = 0.40935 × height + 0.49761 × PAA (P < 0.001, R2 = 0.9965 [adjusted R2 = 0.9965])."
Such "regression" formula has 4 parameters and 4 coefficients: those are too many for something in principle which can be measured directly.
The article does say this:
"...Fetal size is measured by ultrasonography before the delivery. However, the maternal pelvis is not measured before labor, although labor per se has been reported as a way to measure the pelvis."
Passed or not is the clinical test relevantly used, so to say.
Although they measure the interspinous distance directly:
"(5) ISD (narrowest) between the ischial spines;"
Then it gets interesting:
"Second, the height and inlet-AP distance plus PAA (pubic arch angle), which were measurable by intrapartum ultrasound, for measuring ISD were analyzed."
Because:
"The mean ± standard deviation age of the patients was 40.5 ± 6.4 years (range, 21~50 years) and the mean height was 160.1 ± 5.5 cm."
The mean age of women is above usual child bearing age and the stature of 95% of women was below 171.1 cm, so hardly applicable to women who are on average 171.1 cm, of whom half will be taller. Comparing outcomes of 5% vs 50% does not inspire confidence with mere rhetorics.
And it is known pelvic anatomy changes after delivery. Hence a wider pelvis after delivery is a marker of successful vaginal delivery, not the other way around!, at least in non-nulliparous women, at least, but see below. Hence the quoted study is biased, by the average age of the participants.
Although above the sample size calculation, so they said:
"Regarding obstetric history, 245 women had a vaginal delivery, 146 women had a cesarean section, six women had only a stillbirth, and 313 women had no obstetric history"
And the sample is somewhat enriched with women apparently at higher risk of cephalo-pelvic disproportion, so not entirely representative:
"Research has identified a connection between CPD (cephalo-pelvic disproportion) and short maternal height [6, 12], with the majority of the studies based on the cut-off value of 150 cm or <145 cm"
Since 5% of women in their sample will have a stature of 149.1 cm or less.
And even then, it is only 5% of women, too many to have a complication, but to start with too little to be confident, since 5% of 710 women is 36 women. For which “intrapartum” measurements would be available in principle to only 20 women of said stature at or below 149.1 cm.
Hardly of enough size to answer the question I asked: has it been measured relevantly?.
And yeah:
"Interestingly, maternal height was determined to be the most relevant factor in determining ISD in terms of [bony] anatomy in the current study. When comparing the standardization coefficients in the first model, the most determinate factor for ISD was confirmed to be height, rather than any other pelvic component. Hence, expecting that taller mothers will have fewer mid-pelvic contractions is reasonable."
But the field is ripe with false or not really supported findings:
"In the FRABAT study, the PAA in women with vaginal breech delivery was not related to the success of vaginal breech delivery, although vaginal delivery was unsuccessful when the PAA was <70°"
But the Frabat study is hardly applicable: "MRI-based pelvimetric measurements as predictors for a successful vaginal breech delivery in the Frankfurt Breech at term cohort (FRABAT)" does say this "No significant correlation of the intertuberous distance and the pubic angle with the mode of delivery could be shown.", of course for breech deliveries, again hardly applicable to non-breech deliveries, aka normal or normalish deliveries, see below. But hardly a source of confident inspirations since "no significant" correlation was found.
And yet the Frabat was misquoted, apparently: "Although statistically not significant, we were able to define cut-off values of 10.9 cm in the intertuberous distance and 70° in the pubic angle; below these values, no successful vaginal delivery was recorded.", quoted as "...although vaginal delivery was unsuccessful when the PAA was <70° [but not statistically significantly]". Again, the Frabat study was designed to see how better deliver babies when they remain seated instead of going head on with their delivery... in Germany...
And Voilá:
"The results of this study can be thought of as hypothesis generation, and the results are preliminary and further investigation is needed to confirm validity and generalizability for the broader population." [This what they call a defensive statement against lawsuits]
The study they quote ("New MRI Criteria for Successful Vaginal Breech Delivery in Primiparae") as inspiration or basis for their study says this:
"The patients with successful vaginal deliveries were significantly younger than the patients who underwent caesarean section... The neonatal short-term outcomes were comparable in both groups."
Although it does say this:
"The ISD significantly influenced the mode of delivery in the regression analyses."
Vaginal breech is when the baby is up side down!, hardly a study to be based for studying Cephalo-pelvic disproportion!, specially to be used in practice: when delivering babies head on. They quote a 3-4% prevalence of Breech Presentation. Again, hardly a sample to reach conclusion of use for clinical practice, beyond the beware.
Specially because as far as I saw the originally quoted study does not report how many deliveries were attempted in breech, nor how many were present and went to C-Section, obviously suction was not doable, just imaging it gives me goose bumps.
The other study they use for discussion ("Narrow subpubic arch angle [SPA] is associated with higher risk of persistent occiput posterior position at delivery") only included 27/29 women, they say 29, who actually had a "persistent occiput posterior presentation at delivery".
Hardly a sample size big enough.
And in this study the stronger predictions of C-Section or Suction aided delivery were: Prolonged labor, abnormal cardiotocographic findings and a combination of both. Since those are the ones that indicated either the C-Section or the Suction aided vaginal delivery, not some pelvic measurements nor persistent occiput posterior presentation at delivery.
Those three: Prolonged labor, abnormal cardiotocographic findings and a combination of both, were 100% predicting!.
And obviously points at clearly that one of their quoted studies ("Subpubic Arch Angle and Mode of Delivery in Low-Risk Nulliparous Women" had at the minimum mixed findings, hardly conclusive, and its findings were not assessed and published in the originally quoted study.
Suggesting it might be possible they didn´t replicate in the South Korean Population. And it is important because according to the originally quoted study Height and SPA/PAA were the most important predictors.
The study ("Subpubic Arch Angle and Mode of Delivery in Low-Risk Nulliparous Women") did mentioned this: "On the other hand, the duration of labor did not show a significant relationship with SPA.", hence it would not have been one of the indicators for intervention, suggesting bias or confounding in using subpubic arch angle (SPA) measurements with 3D ultrasound close to delivery to predict the outcome of Delivery. And in this study C-Sections or aided vaginal delivery was done on 42.8% of women.
And the SPA and mode of delivery in the supplementary materials, the only thing freely available beyond the abstract, does not show the Height of women, curiously enough, but it does show several other things.
And the Height of the women with persistent occiput posterior presentation at delivery (from the Study "Narrow subpubic arch angle is associated with higher risk of persistent occiput posterior position at delivery") was 160.6 ± 6.0 cm, which is around the same than "160.1 ± 5.5 cm" in the originally quoted study.
Given that, I would have expected more difficulties leading to more C-Sections, but apparently not: 38% (on 4.2 cm taller women on average) v 20.6% (in 4.2 cm shorter women on average). Regardless of presentation at delivery, in both samples as a whole.
And the Study "Narrow subpubic arch angle is associated with higher risk of persistent occiput posterior position at delivery" says this:
"No significant relationship was found between maternal height and SPA", suggesting they are not correlated, and could be independent predictors, perhaps, and from this table it seems SPA has around the same predictive power than Height in the originally quoted study:
And ischial tuberosity distance is around the same too!, even grater than PAA/SPA.
Which seems not that consistent "The most impactful factor was height." At least they might not be linearly correlated.
But understandable because using a different linear regression, a different fit to the data they found this:
So which one is how much more important depends on how the regression was done: based on which model, apparently to support the Hypothesis, the assumption, height was the most important factor despite there was evidence SPA and height were not related, and in the 4 factor regression model they are similar in effects/power, but not in the 2 factor model. A 0.11 v a 0.20 difference in the Standardization coefficient.
But it makes sense: picking among some variables, starting with five, one can pick the model with the biggest difference among two. Despite in the 4 factor model ischial tuberosity distance was a better “predictor” than Public Arch Angle. And the coefficient provides an estimate of their independence among each other: that´s the point of linear regression.
I am going on a limb here, since I am not an expert, but if ischial tuberosity distance has a bigger coefficient in the 4 factor model than PAA, and PAA is not related to height, then how is ischial tuberosity distance related to height?.
There are what?, 10 pairs of variables to pick one pair?: one can pick one among five for the first member of the pair, and then another from among four for the second member of the pair, which is 5x4. But because they can be reversed and it won´t make a difference, one has to divide by two, hence ten pairs instead of twenty.
Which suggests they were looking to publish a positive finding, not to find out the truth.
And in those studies confounding by indication is a consideration.
Then the Study "Narrow subpubic arch angle is associated with higher risk of persistent occiput posterior position at delivery" found a significant difference in Delivery outcomes, "normal" v C-section or aided by suction on a 1.8 cm difference in height on average height between the two groups (165.0 cm minus 163.2 cm, wow! a 1% difference in height!).
I would not call the firepersons on a less than 2cm height difference, representing a 1% difference, among groups of women. Specially because the "transmission" of such small difference in height to pelvic anatomy is probably unmeasurable, even with MRI. Leading, of course, to publication bias.
And the difference in the SPA (the subpubic arch angle) found as significant was 7 degrees, out of a 114 average angle, which is a 6% difference, again, not statistically significantly associated with height.
Which makes sense, statistically significant outcomes are determined, allegedly but hardly credible as general phenomena, on 1% differences in height with 6% differences in angles. On averages among two populations, not among individuals, of course...
Then compare it with the 70 degrees cutoff, a 38.6% difference and the proportions seem quite clear: a 6% difference hardly makes sense as causal for most women individually.
And the significant birth weight difference was 101 grams, or 3% of an average 3358 grams.
So correlating differences in 1% with a 6% and a 3% does lead to publication bias when using regression analysis.
Just think in practice, and I did not saw it reported in the papers I quoted, not of the Standard Deviation of the Mean of the measurements, but the Error in practice, among individuals, not populations. Such requires relevant clinical expertise not provided by merely reading "papers".
The accuracy of the measurement on each individual compared with a Gold Standard. If such a thing even existed for many measurements used in Radiology/Imaging with a basis on non-pathological, not merely based on a “normal distribution”.
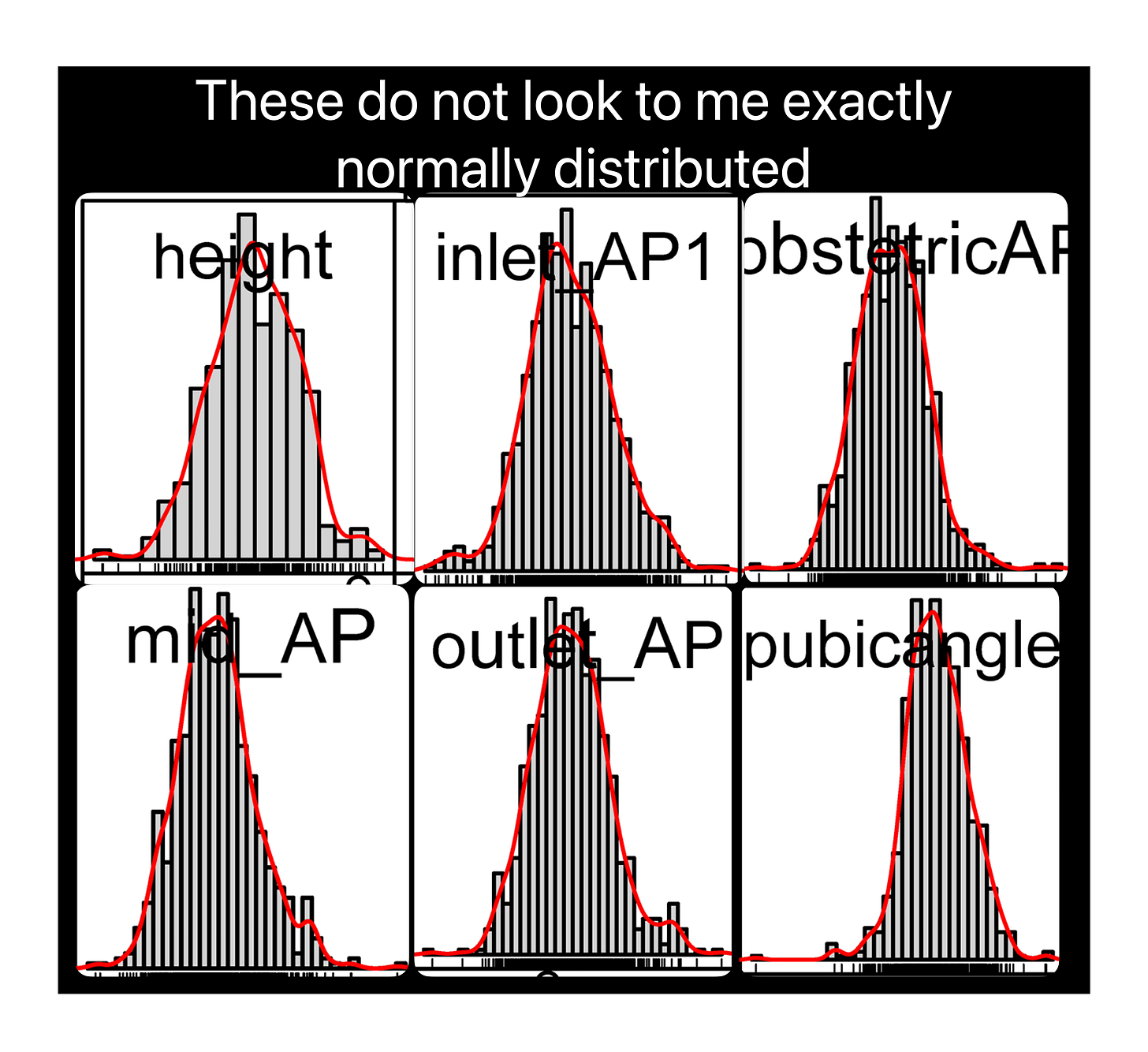
Which by the way, does not look that normal to me, I can see skews in there:
Those small differences: 1%, 3% and 6%, unless at the edges, at the extreme of distributions, and even then Humans being unique, in practice are Fugazis.
Those are small percentage differences at a scale of 164 cm, 114 degree angles and 3358 grams, supposedly correlated with differences in probably the same small percentages at a scale of 11.2 cm, at least an order of magnitude difference!.
Which correspond to 1mm (Height), 4mm (Baby´s Weight), and 7mm (SPA/PAA). Hardly accurate to measure confidently in practice by Clinical Imaging in a Female Pelvis even using MRI… or 3D ultrasound…
And one needs to have trained as a Radiologist to know such small differences are rarely used for making clinical decisions based on Clinical Imaging because although with experience can be seen with the naked eye, Imaging publications are riddled with so many of those "positive" findings which are irrelevant to clinical practice that it is hardly worth reading them...
Unless one is only trying to publish something else or impress someone else, or confuse them, it happens.
As a conclusion to honor the Women I dedicated this Post to:
So in South Korean population being shorter as average of population´s Height leads to around half the risk (52%) of not having a "normal" vaginal delivery, compared to average Height of the Italian Population.
So Height does not look that predictive of having a C-Section or an aided delivery. Which is what I asked, not for some linear regression equations:
"Is there a correlation between height and the size AND geometry of the birth canal, relevant to complications during delivery?." The answer is none was provided. Does not mean none exists, mind you.
And only 4 women in the (160.6 ± 6.0 cm) with a persistent occiput posterior presentation at delivery did not have either a C-Section or an instrumental (aided) delivery. 25 of 29 did. Hence most likely bias or confounding, of several sorts.
So as it goes according to your:
"Science says taller women are biologically superior... I didn’t say it"
Then the statement necessarily follows: South Korean women are superior must be true. As I asked: "...relevant to complications during delivery". I did not asked "related" nor "associated"...
And given South Korean Women in the Studies I referred are shorter by 4.2cm than Italian women, then Height in women related to delivery does not mark superiority.
On the contrary, given Prolonged labor, abnormal cardiotocographic findings and a combination of both are complications of delivery needing intervention then clearly being taller in Italy is worse than being shorter in South Korean, as populations, not as individuals. From the quoted studies, and nothing more. Caveats and all.
Suggesting as Populations South Koreans are Superior to Italians, but such is not supported by the data I saw. And I hate that too…
Sorry, that was not Italian:
Sorry, not that either, but this one makes me cry:
Case closed: one needs to understand what one is reading and not just read the headlines and do selective quotations, Mr. [I got no reply, so blocked].
But for Women, as always, talk to your Caring Health Provider, this is not Medical Advice.
As for me, as in the following Codas, if I was so lucky, the last thing on my mind would be Delivery…
Finally, it was just for show, no factual statements of any sort:
Thanks.
Federico Soto del Alba.